
Dr Leanne Miller is an Occupational Therapist based at the Norfolk and Norwich University Hospital. Here she explains how an accident at the age of 18 months led her to entering a caring profession which helps people with the ‘job of living’
My mum encouraged me visit the Occupational Therapy stand at my high school careers evening as she thought I was would be well suited to a career in one of the ‘caring’ professions. I was 13 at the time and did not know much about OT (or so I thought). I had an idea of what I wanted to do but had struggled to find a career that would encompassed all the aspects I wanted. I had toyed with the idea of joining the police force, contemplated nursing, and looked into physiotherapy.
I walked away from the stand with a beaming smile and finally a title to match the description of my ideal job – it was Occupational Therapy. I later connected that my perfect career had been staring me in the face for years and I just hadn’t realised it!
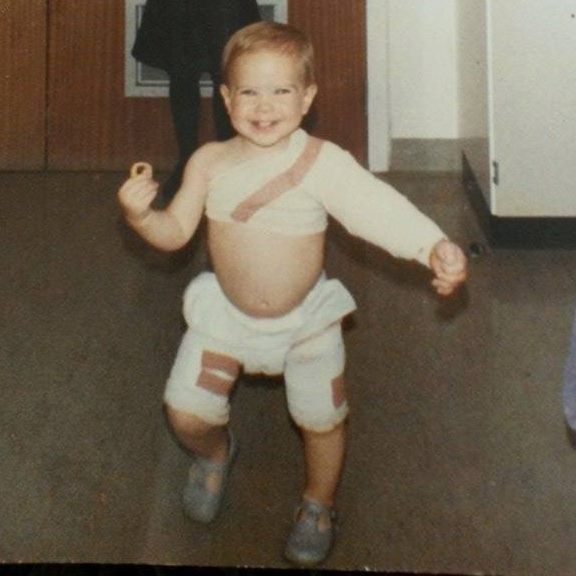
At the age of 18-months-old after an accident at home I sustained full thickness scalds to 9 per cent of my body and in an infant so small this can be very serious. After a month in a regional burns unit, skin grafts, many dressing changes, observations and therapy I was discharged back home following treatment at Royal Preston Hospital.
Throughout this experience, and treatment which spanned 15 years in total, there was only one member of the clinical team who stuck in my mind, who I would ask my mum if we could go and visit and who I looked forward to seeing on my many regular outpatient trips to the hospital – this person was the Occupational Therapist.
The OT measured me up for pressure garments to help flatten the scars, exercises to help regain my arm movement, taught my mum how to massage the scars and helped my mum deal with the emotional impact of my injury. During these sessions the OT used toys, games and food to encourage me to use my affected arm. As I grew older and had to deal with the psychological impact of the scars, bullying at school and the reactions of other people, I became more self-conscious. My OT acknowledged the psychological impact of the injury and how this was affecting my confidence and what I would chose to wear, and she offered me sessions looking at how to camouflage the scars with special make-up.
Despite the trauma which led me to see an OT, I had such positive memories of my treatment sessions and I believe this is due partly to one of the core philosophies of OT: using age-appropriate, meaningful and functional activities to rehabilitate someone back to independence. My OT used play and feeding myself as meaningful activities to me, as an 18-month-old, in order to ensure I used and moved my left arm and hand normally. I have full use of arm and hand now and am confident to wear what I want and to deal with people’s reactions to my scars. Had it not have been for this experience I may never have discovered OT.
I believe that Occupational Therapy is the health care system’s best kept secret, it is often confused with physiotherapy and whilst there is some overlap, OT uses a wide variety of interventions that help people with their daily activities, or the ‘job of living’. Most people do not know what an Occupational Therapist does and the term ‘occupation’ often misleads people to think we focus only on work or employment. In fact, ‘occupation’ encompasses anything that occupies your time (work, self-care, leisure) and an OT can help to overcome barriers preventing you from doing these ‘occupations’. It really is very simple, but often so simple it is overlooked, or indeed undervalued. Occupational Therapists help people of all ages who have, or have had, an illness or injury, either mentally, physically or developmentally which prevents them from balancing or engaging in their ‘occupations’ which are meaningful to them, and which from their sense of identity.
I have been an OT for 16 years now, most of those working with people with hand and upper limb injuries, including burns. I am passionate about this profession, which is so diverse and resourceful in what it can achieve.
I have recently been awarded the only HHE (Health Education England) post-doctoral bridging award/fellowship in the East of England, with the primary aim to develop and submit a competitive NIHR post-doctoral application (Advanced Fellowship). My research focus will be on advanced clinical practice roles within hand therapy and whether these roles improve patient outcomes in a hand trauma setting. This links with the service development project currently being implemented in the department where the finger fracture clinic has now become therapy led.
Working during the pandemic
Working in the NHS during the Covid-19 pandemic has been challenging, information changes daily, sometimes multiple times a day and it hard to keep on top of new information. It has been tiring, mentally draining and has added an extra layer of complexity to our work. As an Occupational Therapist working in an outpatient setting I do not work on the wards so have been, in some ways, sheltered to the direct impact of covid-19, however the virus has changed how the whole hospital functions. Some of my team have been redeployed to the ward and others are working from home because of their own health vulnerabilities.
Our outpatient capacity has been reduced to the absolute essential meaning only urgent post trauma or surgery patients to avoid the footfall coming into the hospital, particularly those who are at higher risk. Where patients would usually come to the hospital for their outpatient therapy appointment, much of this activity has been changed to virtual appointments (video or telephone call). This has meant we have had to learn a new method of delivering our treatment and service, along with web-based systems which are new to us which has been hard for everyone to adapt to. As therapists we rely on face-to-face contact with our patients to build a rapport and to be able to have hands on assessment and treatment and this has not been possible in many cases which has felt like a huge loss. Even wearing PPE can be challenging, it’s hard to communicate effectively with patients when you are wearing a face mask and visor, it’s harder for both parties to hear properly and the non-verbal ques are lost. One-way systems, reduced capacity of clinical spaces, staff testing, and social distancing are now classed as the ‘new normal’ but I don’t think any of us will ever really be used to it.






Leave a Reply